Crosby Health
About Crosby Health
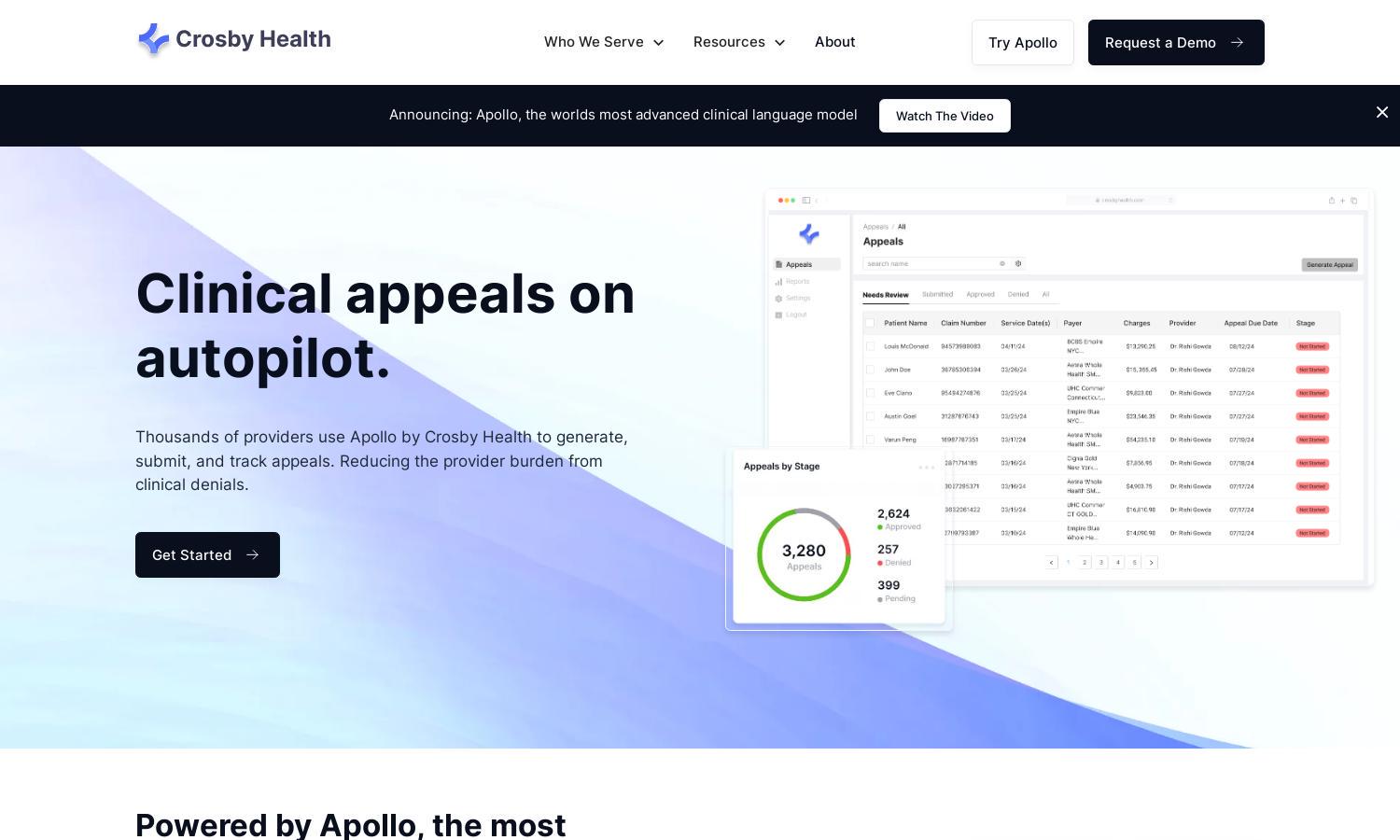
Crosby Health aims to streamline the clinical appeal process for healthcare providers through their AI-powered platform, Apollo. By generating, submitting, and tracking appeals automatically, it alleviates the burden of clinical denials from providers, ensuring quicker recovery and improved efficiency in managing healthcare documentation.
Crosby Health offers various subscription plans to suit different provider needs. Each tier enhances user capabilities, providing comprehensive features for generating appeals. Upgrading offers access to advanced AI functions and specialized support, ensuring better handling of denials and maximizing recovery potential for users.
Crosby Health boasts a user-friendly interface designed for seamless navigation. Its layout simplifies the appeal process with intuitive features, enabling quick access to essential tools. Users can efficiently generate, submit, and track appeals, ensuring that their experience is smooth and effective throughout their engagement with the platform.
How Crosby Health works
Users begin their journey with Crosby Health by signing up for their AI-powered platform, Apollo. After onboarding, they can easily navigate through a user-centric design that highlights key features. The platform allows users to generate appeal letters, submit them to multiple payors with one click, and track the status of each appeal, all while receiving timely notifications and updates.
Key Features for Crosby Health
Automated Appeal Generation
Crosby Health's automated appeal generation is a key feature, leveraging Apollo's AI capabilities to craft precise and compelling denial letters. This unique functionality saves healthcare providers valuable time and effort, ultimately enhancing their chances of securing maximum recoveries on denied claims.
Unified Submission Platform
Crosby Health offers a unified submission platform that allows users to submit appeals to multiple payors with a single action. This feature streamlines the submission process, significantly reducing the complexities involved in managing different payor portals and enhancing operational efficiency for healthcare providers.
Real-Time Tracking and Notifications
Crosby Health provides real-time tracking of submitted appeals, ensuring that users receive immediate notifications regarding the status of their claims. This feature empowers healthcare providers to easily monitor their appeals, facilitating proactive management and timely follow-ups as necessary for optimal recovery outcomes.
You may also like:








